RHEMATOID ARTHRITIS
A 45yr old female came to causality with chief complaints of neck pain , headache and wrist and ankle joint pain since 4 yrs
𝐇𝐈𝐒𝐓𝐎𝐑𝐘 𝐎𝐅 𝐏𝐑𝐄𝐒𝐄𝐍𝐓𝐈𝐍𝐆 𝐈𝐋𝐋𝐍𝐄𝐒𝐒 :-
Patient was apparently asymptomatic 4 yrs ago the she developed fever insidious in onset, not associated with chills and rigor.
𒊹︎︎︎ She developed headache diffuse in nature , not associated with nausea and vomitings since 4 yrs
No H/o cough, cold at the time of fever
𒊹︎︎︎ No H/o giddiness
𒊹︎︎︎ C/o B/L wrist joint paina and ankle joint pains
𒊹︎︎︎ C/o Metacarpo phalanges pain (+)
𒊹︎︎︎ C/o Interphalanges pain (+)
𒊹︎︎︎ C/o Tenderness present over wrist,mcp, Ip
𒊹︎︎︎ H/o fever & episode in last 8months
𒊹︎︎︎ Last episode 20days back
𒊹︎︎︎ Fever last for 1day relieved after taking medication
𒊹︎︎︎ H/o oral ulcer on hard palate since 10days
𝐇𝐈𝐒𝐓𝐎𝐑𝐘 𝐎𝐅 𝐏𝐀𝐒𝐓 𝐈𝐋𝐋𝐍𝐄𝐒𝐒 :-
𒊹︎︎︎ H/o CVA left Up & Ll weakness &slured speech 10 years back
𒊹︎︎︎ H/o Appendectomy 8year back
𒊹︎︎︎ N/k/c/o DM, HTN,TB,Epilepsy,CAD,
𒊹︎︎︎ Used Ayurvedic medication 2 months back for 15days
𝐏𝐄𝐑𝐒𝐎𝐍𝐀𝐋 𝐇𝐈𝐒𝐓𝐎𝐑𝐘 :-
𒊹︎︎︎ Married
𒊹︎︎︎ Occupation -driver
𒊹︎︎︎ Appetite-decrease
𒊹︎︎︎ Mixed diet
𒊹︎︎︎ Bowel- Regular
𒊹︎︎︎ Micturition-normal
𒊹︎︎︎ Habit/addiction
𒊹︎︎︎ Alcohol-toddy dinner since 20yr
𒊹︎︎︎ Occasionall alcoholic
𒊹︎︎︎ BD since 25year (15 per day)
𝐅𝐀𝐌𝐈𝐋𝐘 𝐇𝐈𝐒𝐓𝐎𝐑𝐘 :-
𒊹︎︎︎ No similar complaints in the family.
𝐏𝐇𝐘𝐒𝐈𝐂𝐀𝐋 𝐇𝐈𝐒𝐓𝐎𝐑𝐘 :-
(1) GENERAL HISTORY :-
Height- Weight-
Pallor-absent
Icterus- absent Clubbing-absent
Cynosis- absent Oedema -absent
Lymphadenopathy-absent
No Malnutrition
No Dehydration
𒊹︎︎︎ Vitals:- Temp-Afebrile
Pulse rate -82/min
Respiratory rate-20/min
BP -100/70mmHg
𝐒𝐘𝐒𝐓𝐄𝐌𝐈𝐂 𝐄𝐗𝐀𝐌𝐈𝐍𝐀𝐓𝐈𝐎𝐍 :-
𒊹︎︎︎ CVS - Cardic sound S1&S2 heard
Cardic mummers- No
𒊹︎︎︎ Respiratory system :-No Dyspnoea
No Wheeze
Position of trachea -central
Breath sounds -vesicular(normal)
B/L air entry -Normal
𒊹︎︎︎ Abdomen :- Shape of abdomen - scaphoid
Tenderness-No
Palpable masses- No organomegaly
Liver- Not palpable
Spleen- not palpable
Bowel sounds - yes
Hernial orifices- Normal
𒊹︎︎︎ CNS - level of consciousness -conscious
Speech- Normal
No Signs of meningical irritation ( neck stiffness, kernigs signs)
Cranial nerves-normal
Motor system- normal
Sensory system-normal
Glasgrow scale
𝐈𝐍𝐕𝐄𝐒𝐓𝐈𝐆𝐀𝐓𝐈𝐎𝐍𝐒 :-
𒊹︎︎︎ USG :-
-small shrunken Right kidney with grade-3 RPD changes
- Grade-2 fatty liver with mild hepatomegaly
- Right renal cortical cyst
𒊹︎︎︎ 2D ECHO :-
- Good LV systolic function
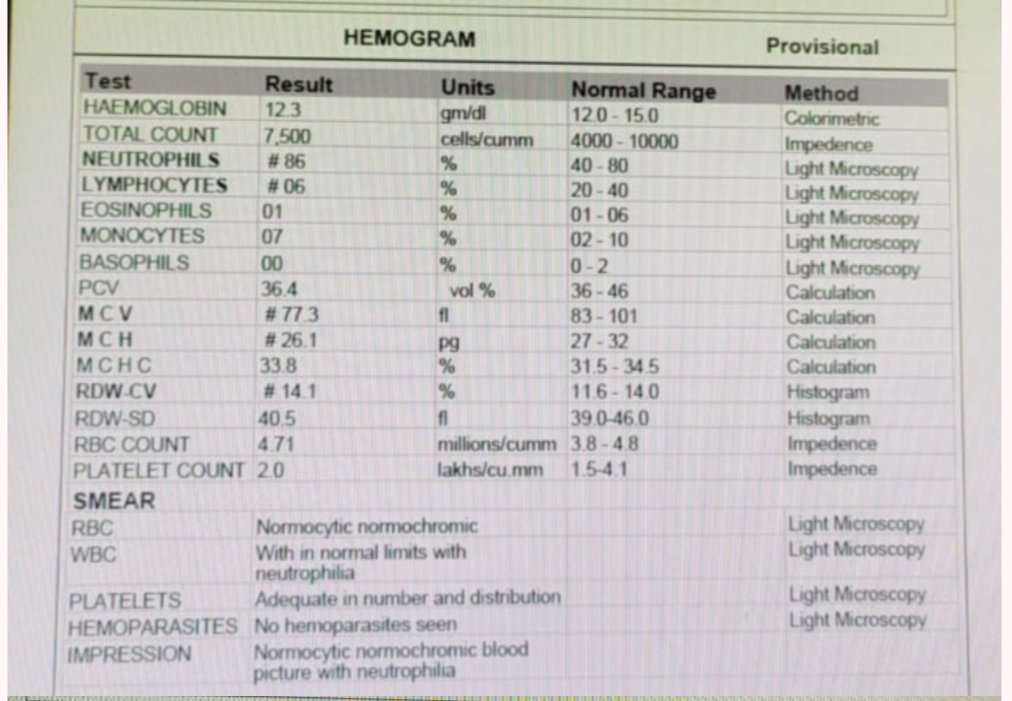
𒊹︎︎︎ HAEMOGRAM -
𝐏𝐑𝐎𝐕𝐈𝐒𝐈𝐎𝐍𝐀𝐋 𝐃𝐈𝐀𝐆𝐍𝐎𝐒𝐈𝐒 :-
𝙎𝙔𝙎𝙏𝙀𝙈𝙄𝘾 𝙇𝙐𝙋𝙐𝙎 𝙀𝙍𝙔𝙏𝙃𝙀𝙈𝘼𝙏𝙊𝙐𝙎
𝐓𝐑𝐄𝐀𝐓𝐄𝐌𝐄𝐍𝐓 :-
- MUCOPAIN GEL- thrice daily
- T. PCM-650 - thrice daily
- T.BENFOMET PLUS- once daily
- T.PREGABALIN- once daily
- T.BACLOFENX-L- once daily
- T.LORAZEPAM - once daily
- T.NICOTINE GUMS- twice daily
- T. HCQ-200mg/BD
𝐀𝐃𝐕𝐈𝐂𝐄 :-
No active intervention Needed from nephrology